With so much detailed knowledge and advanced technology in the field of medicine, it’s easy to become laser focused on one’s own specialty. This, however, can lead to tunnel vision and bias which in turn may lead to misdiagnosis and/or delayed treatment. Dermatologists, especially,
know that “if your only tool is a hammer, everything begins to look like a nail.” Perhaps we are more acutely aware of the need for cross-disciplinary training because very rarely does a patient present with a skin issue that is “just” a skin issue.
Take hidradenitis suppurativa (HS), for example. Besides an apparent link to obesity and smoking, it has an association with arthritis, diabetes, metabolic syndrome, and inflammatory bowel disease. As a review on HS in JAAD International put it, “Observational, experimental, and therapeutic evidence supports the concept of hidradenitis suppurativa as a primarily inflammatory disorder, a disorder of autoimmunity, or both, in contrast to the current prevailing paradigm of primary follicular occlusion.”
Masterclasses in Dermatology is a unique educational experience because we offer interdisciplinary education from experts in multiple therapeutic areas like gastroenterology, rheumatology, dermatology, surgery, and ophthalmology. In fact, two of our co-chairs, Dr. Alice Gottlieb and Dr. Joseph F. Merola, believe so strongly in the importance of cross-discipline education, they have completed two separate residencies, one in dermatology and one in rheumatology. It’s no wonder that they will be leading discussions titled “What’s New in HS?” and “HS Co‐morbidities” at our next Masterclasses in Dermatology from 2/23/23 to 2/26/23. See our full agenda for these and other exciting topics.
Hidradenitis Suppurativa
Like most autoimmune/inflammatory diseases, the cause of hidradenitis suppurativa is unknown. What triggers these boil-like lumps, blackheads, cysts, scarring, and sinus tracts that leak malodorous pus is the subject of much debate and research. And for good reason! Left untreated, the lumps can become quite painful and extensive. Particularly among physician-resistant patients, they are easily dismissed at first, especially since they generally first appear in hard-to-see places.
Many patients report hoping that the lumps will resolve on their own with improved hygiene, like with pimples or ingrown hairs. They also report embarrassment if they first appear in the groin or between the buttocks. Why hair follicles in areas of skin-on-skin contact areas such as the armpits, breasts, and groin are primarily affected is one of the mysteries of hidradenitis suppurativa. Sex hormones are implicated because it is less common before puberty and after the menopause. Many people with the condition also have acne and hirsutism. And like many autoimmune/inflammatory diseases, hidradenitis suppurativa appears to have a genetic component, with about a third of patients reporting that it runs in their families. HS has profound negative effects on patients’ quality of life, which often culminate in social withdrawal, unemployment, depression and suicidal thoughts. About the only good news regarding this maddening disease is that it’s not infectious.
The authors of The Most Recent Advances in Understanding and Managing Hidradenitis Suppurativa touch on a multidisciplinary aspect of HS that is not encouraging; in fact it is rather alarming! Only about half of HS patients receive their diagnosis from a dermatologist, the rest being from general practitioners or non-dermatologists. At first blush, this sounds positive: non-dermatologist physicians are identifying the presence of HS. However, they point to a study that purports that nearly two-thirds of sufferers visited a physician five times or more before getting a proper diagnosis. In fact, nearly 20% of the study participants reported having visited an emergency department more than five times, and that over 10% reported having been hospitalized for HS symptoms more than five times!
As we mentioned, at Masterclasses in Dermatology, we are working hard to create cross-disciplinary awareness. We are painfully aware of the need to address the tunnel vision that would allow a person to be seen in a hospital setting multiple times without their HS symptoms being recognized. And lest it sound like we’re casting dispersions on our colleagues, dermatologists are not above reproach. The authors of the above article note that over the past twenty years, the vast majority of hidradenitis suppurativa related articles were published solely in dermatology journals.
In other words, most of us need an extra level of discipline when it comes to communicating with other disciplines!
Comorbidities of Hidradenitis Suppurativa
The comorbidities of HS include metabolic and cardiovascular disorders, which contribute to reduced life expectancy. A Journal of Dermatology Therapy article, Review of Comorbidities of Hidradenitis Suppurativa: Implications for Daily Clinical Practice, discusses many of the debilitating comorbidities of HS, such as:
- Increased Cardiovascular (CV) Disease Risk
- Axial Spondyloarthritis
- Inflammatory Bowel Disease
- Psoriasis
- Alopecia areata
- Vitiligo
- Pyoderma gangrenosum
- Rheumatoid arthritis
- Non-melanoma skin cancer
- Working Disability
- Psychological Comorbidity
“Working disability,” according to the article, is prevalent in HS patients. The authors relay a study that found that over half of sufferers reported that the disease caused a significant level of work absenteeism. Many experience a substantial economic burden due to either healthcare costs and/or job loss. In general, HS patients have more total work loss days, higher annual total indirect costs, and lower annual income compared with controls.
“Psychological Comorbidity,” the authors point out, is a substantial burden for those with HS. Sexual dysfunction, opioid abuse, and suicidal ideation are some of its extremely consequential effects. Quality of life in HS patients has been found to be more negatively impacted than with psoriasis, acne, stroke, or even with heart transplant candidates. It’s easy to see how HS symptoms can lead to sexual dysfunction and relationship dissolution. The shame and irritation related to the smell, scars, itching, and pain can cause low self-confidence, depression, and social isolation. These results, the authors believe, reinforce the need to assess a patient’s Dermatology Life Quality Index (DLQI) and take sexual health into account when assessing disease severity, response to treatment, and patient goals of care.
Managing Hidradenitis Suppurativa
The authors of The Most Recent Advances in Understanding and Managing Hidradenitis Suppurativa touch on the challenges of researching HS due to its multidisciplinary nature. They discuss the fact that differing presentations between men, women, and different ethnic groups, as well as a lack of standardized language for grading HS severity and symptom presentation, have hampered clinical trials. Our co-chair, Dr. Gottlieb, mentioned earlier, recognizes this issue and is involved with standardizing the numerous and diverse reported outcome measures. In fact, she is a contributing author of Protocol for the Development of a Core Domain Set for Hidradenitis Suppurativa Trial Outcomes. However, despite these difficulties, a greater understanding of HS pathogenesis is leading to the development of targeted topical, oral, and injectable therapies.
Unfortunately, surgery remains one of the top options for managing hidradenitis suppurativa because of the delay in treatment seeking as well as missed diagnosis opportunities. Patients who have developed sinus tracts typically require surgery, the primary goals of which are removal of the diseased tissue and prevention of recurrence.
Cryoinsufflation, injecting liquid nitrogen directly into the sinus tracts, shows promise in helping delineate them prior to carbon dioxide laser excision. Cryoinsufflation could also be used prior to other surgical procedures in HS including deroofing and limited and radical excision. Fortunately, cryoinsufflation is relatively simple and rapid to perform, and most dermatology clinics already have liquid nitrogen readily available.
Non surgical therapies are available and offer some hope to HS patients.
- Topical and systemic antibiotics: Doxycycline, clindamycin, rifampin. Patients with severe symptoms might need to take antibiotics for months.
- Hormone therapy: estrogen-containing combined oral contraceptives (Estrace, Prefest), might be effective for people with mild hidradenitis suppurativa.
- Steroid injections: For mild cases, steroid injections can give patients relief. Triamcinolone (Aristospan, Kenalog-10) injected into the sores might help reduce swelling and inflammation.
- Antiandrogens: Finasteride and Spironolactone have been used to treat many dermatologic conditions. Limited data from small studies and clinical usage has shown positive results for severe cases of HS.
- Biguanides: Metformin, an oral hypoglycaemic agent, may play an important role in delaying or preventing the onset of diabetes and metabolic syndrome; it has been reported as having efficacy in HS.
- Retinoids: commonly used to treat acne and inflammatory skin conditions, they can be effective in treating the symptoms of hidradenitis suppurativa as well.
- Fumarates: For especially therapy-resistant cases.
An article in Journal of Drugs in Dermatology, Hidradenitis Suppurativa: Review of the Pathogenesis and Treatment, co-authored by Dr. Gottlieb, discusses many of the above therapies. It also discusses immunosuppressive drugs, because if other treatments are ineffective, but the HS symptoms are caught early enough, immunosuppressive therapy is an option.
Tumor necrosis factor (TNF) inhibitors adalimumab and infliximab are two of the most promising options. Several of these drugs are approved for the treatment of moderate to severe hidradenitis suppurativa and many others are in clinical trials. Table 1 “Summary of immunomodulatory therapies reported in the treatment of hidradenitis suppurativa” from The Most Recent Advances in Understanding and Managing Hidradenitis Suppurativa is reproduced below:
TNF-alpha
- Adalimumab
- Infliximab
- Etanercept
- Golimumab
- Certolizumab
IL-1 inhibitors
- Anakinra
- Bermekimab
- MEDI8968 (NCT 01838499)
IL-17 inhibitors
- Secukinumab
- Bimekizumab
- Ixekizumab
- CJM112 (NCT 02421172)
IL-12/IL-23 inhibitors: Ustekinumab
IL-23 inhibitor: Guselkumab
Complement C5a inhibitor: IFX-1
LFA-1: Efalizumab
CD20 inhibitor: Rituximab
Other systemic immunomodulators
Dihydrofolate reductase inhibitor: Methotrexate
Calcineurin inhibitor: Cyclosporine
ATRA prodrug: RXR/RAR: Acitretin
nuclear transcription factors: Isotretinoin
Reduction in superoxide production and neutrophil function: Dapsone
PDE4 inhibitor: Apremilast
JAK-1 inhibitor : INCB054707
Lifestyle Changes
No one ever really wants to hear it, but unfortunately we need to be assertive with our patients regarding certain risk factors that they have some control over.
- Obesity: Being overweight is implicated in many health issues. HS sufferers, especially, should be encouraged to lose weight if they are obese.
- Smoking: A strong link between and smoking and exacerbation of HS symptoms exists. As another lifestyle choice implicated in a plethora of health issues, patients with hidradenitis suppurativa should be strongly urged to quit smoking.
- Diabetes: Although diabetes isn’t a lifestyle “choice,” vigorously managing one’s diabetes symptoms is highly recommended for those with HS.
- Hygiene: Patients should avoid shaving affected areas and avoid wearing perfume or perfumed deodorants.
- Support: Patients should be encouraged to seek outside support and/or mental health counseling to help with coping, especially those with sever symptoms. The Hidradenitis Suppurativa Trust, can also provide help and support.
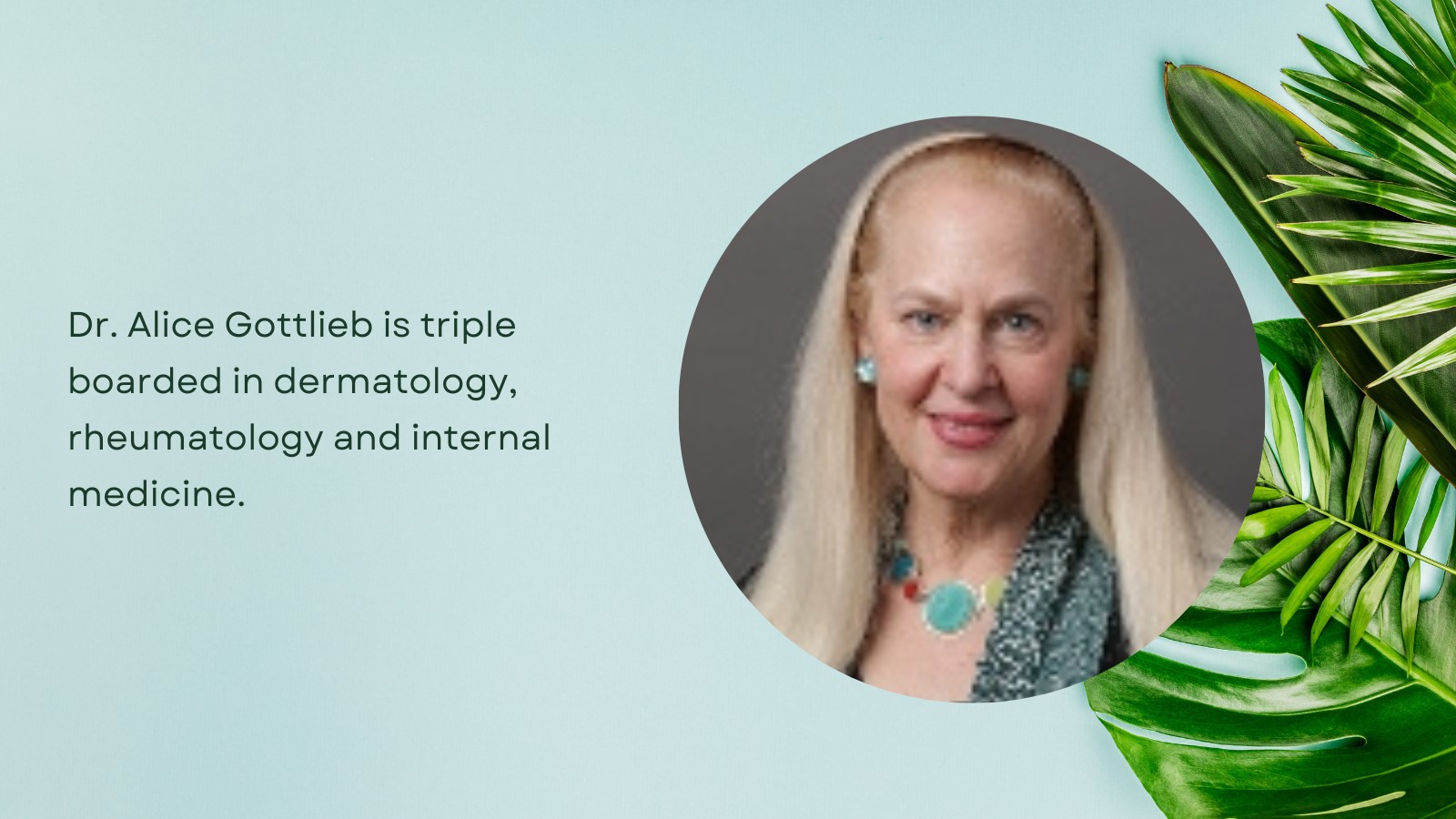
Meet Dr. Gottlieb
As we mentioned earlier, co-chair of Masterclasses in Dermatology, Dr. Gottlieb MD, PhD is a rheumatologist as well as a dermatologist. She is triple boarded in dermatology, rheumatology and internal medicine, making her one of only a handful of doctors in the United States to be certified in all three specialties. She is Medical Director, Mount Sinai Beth Israel Dermatology, Kimberly and Eric J. Waldman Department of Dermatology at The Icahn School of Medicine at Mount Sinai, and contributes extensively to research in the fields of dermatology, rheumatology, and interdisciplinary collaboration.
Dr. Gottlieb founded the Tufts Dermatology residency program and served as Chair of Dermatology and Dermatologist-in-Chief of Tufts Medical Center. She also founded the Dermatology Division at UMDNJ-Robert Wood Johnson Medical School where she served as Professor of Medicine, Director of the Clinical Research Center and Founding Director of the Psoriasis Center of Excellence. Before joining the Mt Sinai faculty, she was a Professor of Dermatology at New York Medical College in New York City.
Dr. Gottlieb is an internationally recognized expert in the field of psoriasis and psoriatic arthritis. She was the first to show the efficacy of TNF blockers as monotherapy for moderate to severe psoriasis. Her research led to multiple TNF blockers being FDA-approved for psoriasis which revolutionized the care of psoriasis and psoriatic arthritis patients. Additionally, she has presented her research at more than 300 dermatology and rheumatology conferences in Asia, Europe and the United States, as well as the FDA and the National Academy of Sciences.
Dr. Gottlieb has served on the editorial boards of numerous peer-reviewed journals. And due in part to her intense interest in interdisciplinary collaboration, she founded and is President of the International Dermatology Outcome Measures (IDEOM) group. This consortium of patients, physicians, and pharmaceutical scientists seeks to standardize the language and protocols of dermatological clinical studies which would greatly increase sharing of data and therapeutic advances.
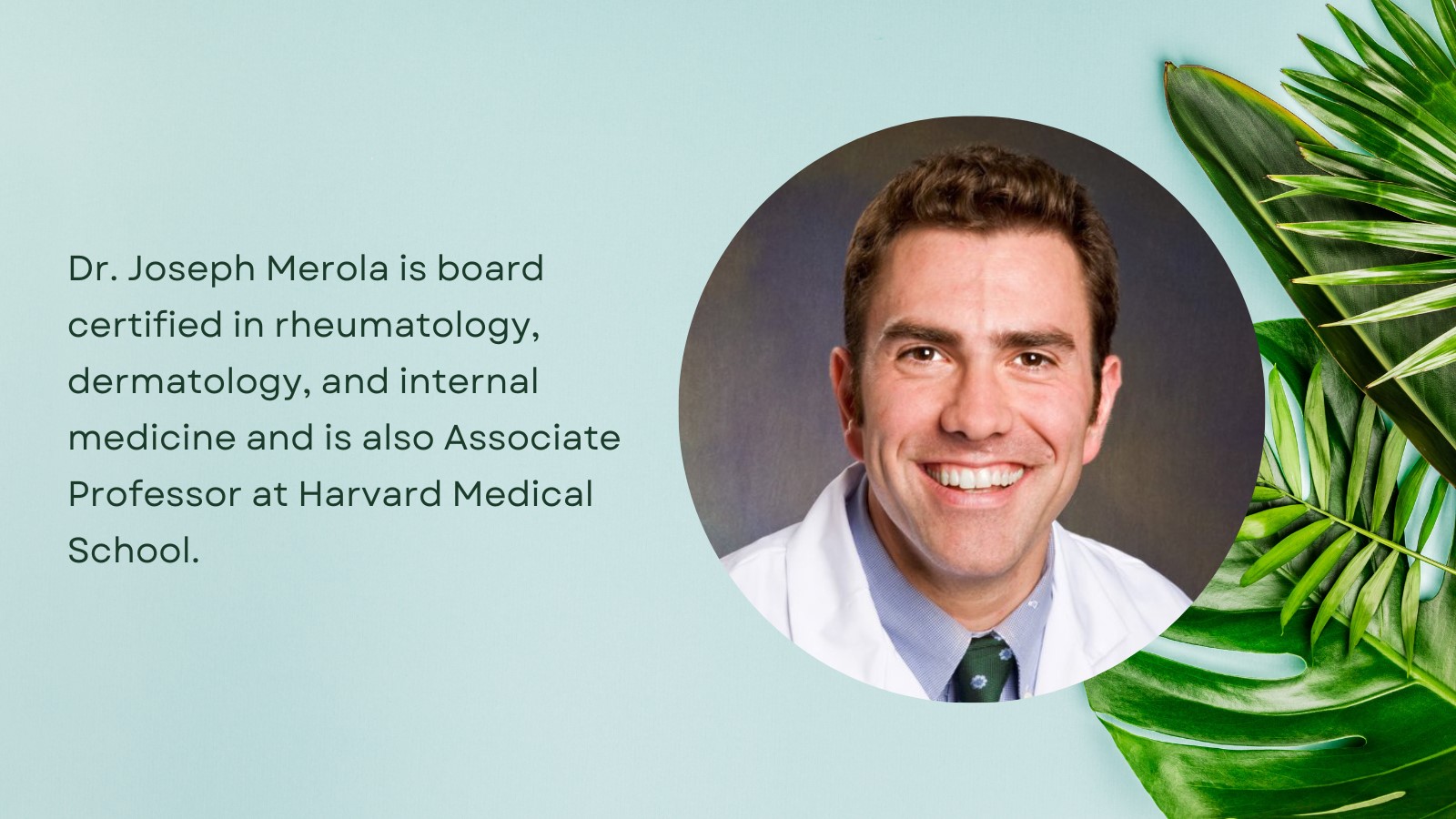
Meet Dr. Joseph Merola
Another of our co-chairs, Dr. Joseph Merola, will be also be leading a discussion on the comorbidities of HS. Like co-presenter Dr. Gottlieb, Dr. Merola is also passionate about cross-disciplinary education and leadership. He is board certified in rheumatology, dermatology, and internal medicine. Dr. Merola is also Associate Professor at Harvard Medical School.
As Director of the Clinical Unit for Research Innovation and Trials (CUReIT), he supports observational and interventional clinical studies across the breadth of the development spectrum. This program offers a unique opportunity for translational research that includes clinical outcome measure development, study consulting, and trials that support proof-of-concept through registrational / Phase III studies and post-marketing registry and phase IV endeavors. They are able to utilize central Institutional Review Board (IRB) for a subset of industry-sponsored studies and master agreements are often in place to facilitate study startup.
He is also Director of the Center for Skin and Related Musculoskeletal Diseases; Associate Program Director, Harvard Combined Internal Medicine-Dermatology Residency Training Program; Vice Chair of Clinical Trials and Innovation, Department of Dermatology; and has authored or co-authored 224 peer-reviewed articles.
Besides discussing developments is treating hidradenitis suppurativa, he will be leading sessions on PsA for the Dermatologist; What’s New in Psoriatic Arthritis?; and Systemic Lupus for the Dermatologist at our next Masterclasses in Dermatology.
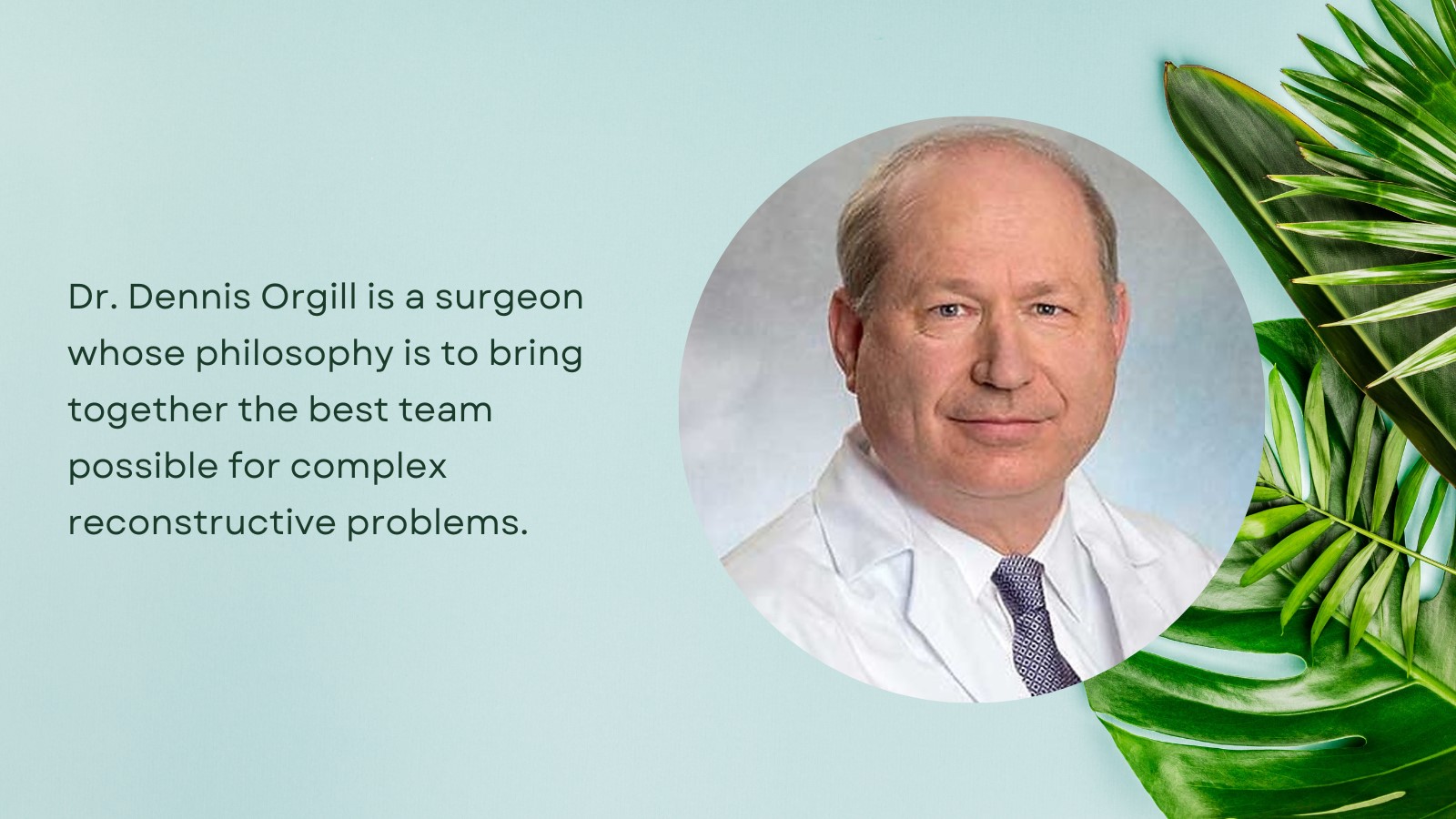
Meet Dr. Dennis Orgill
In keeping with Masterclasses in Dermatology’s belief in multidisciplinary medicine, we would like to present Dr. Dennis Orgill. He is a surgeon whose philosophy is to bring together the best team possible for complex reconstructive problems. This frequently includes both surgical and medical experts from various fields.
As mentioned earlier, surgical intervention is often necessary for hidradenitis suppurativa patients. Dr. Dennis Orgill will be discussing Surgical Management of HS next year in Sarasota at our next session. He is a reconstructive plastic surgeon, Medical Director of the Wound Care Center at Brigham and Women’s Hospital, and Professor of Surgery at Harvard Medical School. Dr. Orgill has a particular clinical interest in complex adult reconstructive procedures including treating complex wounds.
Dr. Orgill has a PhD from MIT in Medical Engineering and runs a tissue engineering and wound healing laboratory at Brigham and Women’s Hospital. His research is focused on developing better technologies to treat wounds including work with artificial skin, micromechanical forces, platelets, and stem cells. He has consulted for several medical device and start-up companies and is the holder of several patents. He worked on the team that developed Integra, a skin replacement therapy that has been commercially developed and used successfully on thousands of patients.
Join Us in February in Beautiful Sarasota, FL
Our next dermatological conference will take place in person at the Ritz-Carlton in Sarasota, Florida on February 23-26, 2023 and will, of course, include diagnosis and treatment of chronic inflammatory skin diseases including hidradenitis suppurativa. There have been many innovations in dermatology in 2022 and you don’t want to miss a single one of our dermatology classes!
You can register for the next Masterclasses in Dermatology on our registration page. You can check out our full agenda on our website and see who our faculty is, who our exhibitors will be, and learn what CME credits will be available.
All meeting and meal functions will be held at the beautiful The Ritz Carlton Sarasota, but many nearby hotels such as The Westin and Art Ovation are just a short walk away from the meeting venue! Enjoy the sunshine and kick your feet up after an exciting day of learning and networking!